Medial Collateral Ligament (MCL) Injuries
What Is the Medial Collateral Ligament?
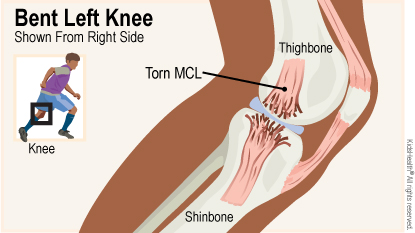
The medial collateral ligament (MCL) is one of the ligaments in the knee joint. A ligament is a tough, flexible band of tissue that holds bones and cartilage together.
The MCL is on the part of the knee closest to the other knee (the "medial" side). It connects the bottom of the thighbone (femur) to the top of the shinbone (tibia). The MCL helps keep the knee from moving side to side.
What Is a Medial Collateral Ligament Tear?
The MCL can tear if an injury stretches it too much. The tear might be partial (through a part of the MCL) or complete (all the way through the MCL).
What Are the Signs & Symptoms of a Medial Collateral Ligament Tear?
Most people who tear their MCL feel pain and a "pop" in their knee when the injury happens. Their knee usually swells soon after the injury, most of the time around the inside part of the knee.
After the swelling goes down, a person usually can walk, but feels pain when the inside of the knee is stretched, Also, the knee may feel unstable and can "give way" and make the person stumble or fall.
What Causes Medial Collateral Ligament Tears?
Most medial collateral ligament tears happen during athletic activity, such as when someone:
- changes direction or twists the knee while running
- jumps and lands in a way that twists the knee
The MCL also can tear if the knee is hit forcefully from the side.
Who Gets Medial Collateral Ligament Tears?
MCL tears happen most often during sports involving turning, cutting, and pivoting like skiing, soccer, football, basketball, and tennis.
How Is a Medial Collateral Ligament Tear Diagnosed?
To diagnose a torn MCL, health care providers ask about the injury and do an exam. During the exam, the health care provider presses on the knee and legs and moves them in certain ways. This can help show if the MCL is torn.
Imaging tests done can include:
- X-rays to check for injuries to the bones
- sometimes, an MRI to check if the tear is partial or complete and to see if the knee has other injuries
How Is a Medial Collateral Ligament Tear Treated?
Right after the injury, the initial treatment may include:
- over-the-counter pain medicine such as acetaminophen (Tylenol® or store brand) or ibuprofen (Advil®, Motrin®, or store brand)
- RICE: Rest, Ice, Compression (with an elastic bandage), and Elevation (raising the knee)
- bracing: your provider will advise you about the best type of brace to protect the MCL and the knee joint during healing.
Other treatments may include:
- using crutches during recovery
- physical therapy (PT) to help with strength and flexibility
- surgery
Can Someone With a Torn MCL Play Sports?
Teens with a torn MCL usually need to take time off from sports, especially the sport in which the injury happened. If there is no pain and the knee does not "give way," they can usually walk, stretch, and do low-impact activities such as swimming.
Teens with a torn MCL should follow their health care provider's instruction on which activities they can do and which they should skip. Most teens with a low-grade MCL tear are back to sports within 6 weeks.
Are There Ways to Help Prevent Another MCL Tear?
Having an MCL tear puts someone at higher risk for another one. To lower the risk of another MCL tear or other injury, work with a physical therapist or trainer to:
- improve your strength, balance, and flexibility
- learn the proper techniques for jumping, landing, and changing direction while playing sports
How Can I Feel Better?
Recovering from an MCL tear takes time. It's normal to feel angry, frustrated, or down, especially if you can't play a sport you love. To stay involved in sports during recovery, you can be part of the team by keeping score or being a manager.
Maybe you can try something other than sports, like playing a musical instrument, painting, or drawing.
While the MCL tear heals, follow your health care provider's instructions for:
- follow-up visits
- physical therapy appointments
- not doing activities that can slow healing
- doing at-home exercises
Reviewed by: Alvin Wei-i Su, MD
Date Reviewed: Jun 17, 2019
















