Hypoplastic Left Heart Syndrome (HLHS)
What Is Hypoplastic Left Heart Syndrome (HLHS)?
Hypoplastic left heart syndrome (HLHS) is a problem that happens when the left side of a baby’s heart doesn't form as it should. It’s smaller than normal and can’t pump enough blood to the body. After the baby is born, doctors can treat the problem with medicines and several surgeries. Some babies will need a heart transplant.
How Does the Heart Work?
The heart is a pump with four chambers. At the top are two atria (the right atrium and left atrium). Below them are two ventricles (the right ventricle and left ventricle).
- The blood flows from the body into the right atrium.
- Then it flows into the right ventricle and gets pumped through the pulmonary artery to the lungs.
- The blood picks up oxygen in the lungs, then travels through the pulmonary veins to the left atrium.
- Blood flows from the left atrium to the left ventricle.
- The left ventricle pumps blood out through the aorta to the body to deliver the oxygen.

90 Second Summary: Hypoplastic Left Heart Syndrome
Learn the basics in 90 seconds.
What Happens in Hypoplastic Left Heart Syndrome?
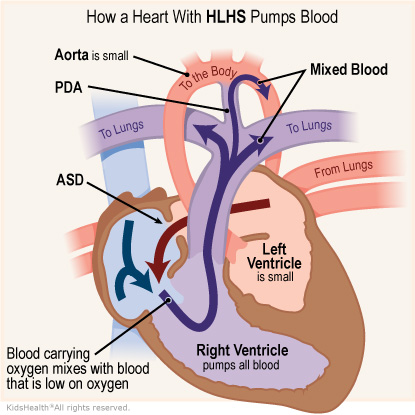
In hypoplastic left heart syndrome, the left ventricle is too small. The aorta, which takes the blood to the body, is small too. The heart can’t pump enough blood to the body.
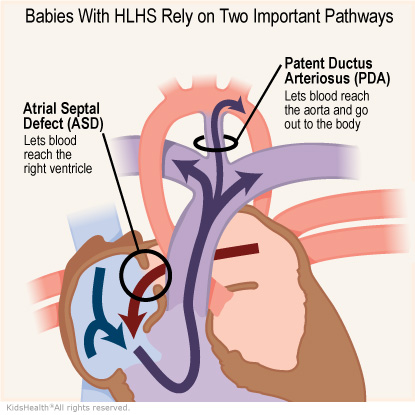
The right ventricle, which is only supposed to pump blood to the lungs, pumps blood to the lungs and the body through a connection called a patent ductus arteriosis (PDA). Usually, babies don’t need this connection after they’re born so it closes. But a baby with hypoplastic left heart syndrome needs this connection to get blood to the body. Because the right ventricle is pumping blood to the lungs and the body, it is doing extra work.
Babies with HLHS are almost always born with an atrial septal defect (ASD). This is a hole between the atria that lets blood with oxygen mix with blood low on oxygen. This way, the blood that the right ventricle pumps out to the body has some oxygen in it.
What Are the Signs & Symptoms of Hypoplastic Left Heart Syndrome?
A baby born with hypoplastic left heart syndrome may have:
- fast breathing
- blue or grayish coloring of the skin and nails
- trouble feeding
- low energy and activity
- fewer than normal wet diapers
What Causes Hypoplastic Left Heart Syndrome?
HLHS is a birth defect that happens when a baby is growing in the womb. No one knows exactly what causes it, but it could have a mix of causes, including a baby's genes (DNA).
How Is Hypoplastic Left Heart Syndrome Diagnosed?
Doctors sometimes can diagnose hypoplastic left heart syndrome before a baby’s birth if the problem is seen on the mother’s prenatal ultrasound scan.
If a baby is born with signs of the condition, doctors do tests such as:
- chest X-ray
- electrocardiogram (ECG or EKG)
- echocardiogram
- pulse oximetry
- blood tests
How Is Hypoplastic Left Heart Syndrome Treated?
To treat most babies with hypoplastic left heart syndrome, doctors:
- Give medicine called prostaglandin to keep the ductus arteriosus open so the right ventricle can continue pumping blood out to the body.
- Do three surgeries: the Norwood procedure, Glenn procedure, and Fontan procedure. These are done in order, and start in the first 2 weeks of life, before a baby goes home from the hospital.
Some babies also may need:
- medicine to help balance how much blood goes to the lungs and how much goes to the body
- a feeding tube that goes in the nose down to the stomach
- cardiac catheterization or surgery to make the ASD bigger. This lets more blood with oxygen flow from the left side of the heart to the right side of the heart.
How Can Parents Help?
Learn as much as you can about hypoplastic left heart syndrome and the treatments your child needs. This will help you work with the care team and better help your child cope. Be sure to ask when you have questions. You can also learn more online at:
You play a big role in your child's treatment. Keep a record in a notebook or in your phone of:
- your child’s appointments, medicines, and any symptoms
- any special instructions for taking care of your child at home
- any questions you have for the care team
What Else Should I Know?
Children with hypoplastic left heart syndrome need intensive medical care from birth. They’ll have many follow-up doctor visits and tests, as well as surgery. At times this might feel overwhelming. You don't have to go it alone. The doctors, nurses, social workers, and other members of the care team are there to help you and your child. Talk to any of them about resources that can help your family.
Take time to take care of yourself too. Parents who get the support they need are better able to support their children.
It can help to find a support group for parents of children with serious heart conditions. Ask the care team for recommendations. You also can look online at:
Reviewed by: Christian Pizarro, MD
Date Reviewed: Apr 26, 2021
















