Pinworm Infections
What Are Pinworms?
Pinworms are tiny worms that can cause an infection in the intestines. Pinworm infections affects millions of people each year, especially school-age kids
If your child develops a pinworm infection, try not to worry. Pinworms don't cause any harm (just itching and restless sleep), and it won't take long to get rid of them.
How Do Pinworm Infections Spread?
Pinworm infections are contagious. The worms get into the body when people swallow the tiny pinworm eggs. The eggs can be on contaminated hands, under fingernails, and on things people touch a lot, such as:
- clothing, bed linens, and towels
- bathroom surfaces
- drinking glasses and eating utensils
- toys
- kitchen surfaces
- desks or lunch tables at school
Less often, eggs can spread when someone shakes out contaminated clothing or sheets, sending the eggs into the air, where they can get inhaled.
The eggs pass into the digestive system, where they hatch. About 1 to 2 months later, adult female pinworms lay eggs on the skin right around the anus, which makes the area itchy. Often, this happens at night.
When someone scratches the itchy area, tiny pinworm eggs get on their fingers. Contaminated fingers can then carry pinworm eggs to the mouth, where they go back into the body, or onto touched surfaces, where they can live for 2 to 3 weeks.
Family pets can't give your child an infection, as pinworms don't come from animals.
What Are the Signs & Symptoms of Pinworm Infection?
Common signs of a pinworm infection are:
- itching around the anus (especially at night)
- trouble sleeping
- vaginal discharge in girls, if pinworms spread to the vagina
- sore, red infected anal skin (which can happen from scratching)
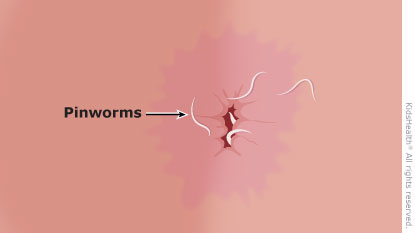
- tiny white worms (like a piece of thread, as big as a staple):
- around the anus (check after your child has been asleep for 2–3 hours)
- in the toilet or on the toilet paper after your child goes to the bathroom
- in the underwear in the morning
Belly pain and nausea are less common symptoms but can happen if there are many pinworms in the intestines.
How Are Pinworm Infections Diagnosed?
The doctor will ask questions about your child’s symptoms and check your child’s bottom. The doctor may ask you to help make the diagnosis of pinworms by doing a tape test:
- Press the sticky side of a piece of clear tape against the skin around your child's anus at night or when they first wake up (pinworm eggs will stick to the tape).
- Wash your hands.
- Take the tape to the doctor to check for eggs with a microscope.
The doctor also might take some samples from under a child's fingernails to look for eggs.
How Are Pinworm Infections Treated?
If your child has a pinworm infection, the doctor will recommend an over-the-counter or prescription antiworm medicine. This is given in one dose, then repeated in 2 weeks. The doctor may decide to treat the entire family, especially if your child has had a pinworm infection before.
Although medicine takes care of the worm infection, the itching may continue for about a week. So the doctor also might give your child a cream or other medicine to help stop the itching.
Can Pinworm Infections Be Prevented?
When someone in the house has a pinworm infection, it often spreads to others.
To help prevent a pinworm infection from spreading in your family:
- Remind kids to wash their hands well and often, especially after using the toilet, after playing outside, and before eating.
- Keep kids' fingernails short and clean.
- Make sure your kids shower or bathe every day. Doing so in the morning can help wash away any eggs.
- Change and wash underwear and pajamas daily.
- Wash towels, clothes, and sheets in hot water often (daily, if you can).
- Tell kids not to scratch around their bottom or bite their nails.
When Should I Call the Doctor?
Call the doctor if your child complains of itchy skin or always seems to be scratching the anal or vaginal area.
Also ask if pinworms could be why your child has trouble sleeping or has begun to wet the bed. (Pinworms can irritate the urethra — the tube through which pee leaves the body — and lead to bedwetting.)
Remember that pinworms are quite common among kids and aren't harmful. By taking medicine and following some prevention tips, you'll be rid of the worms in no time.
Reviewed by: Melanie L. Pitone, MD
Date Reviewed: Nov 5, 2022
















