Basilar Invagination
What Is Basilar Invagination?
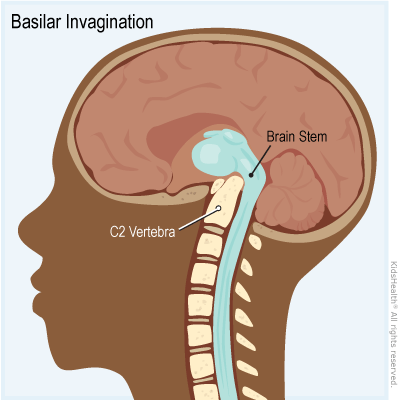
Basilar invagination (BI) is when the top of the spine pushes into the base of the skull. This causes pinching and pressing on the brain stem, the thick bundle of nerves that connects the brain to the spinal cord.
Basilar invagination (BA-zih-ler in-vaj-ih-NAY-shin) that is mild is called basilar impression.
What Happens in Basilar Invagination?
The condition is caused by either an unusual flattening of the bottom of the skull (called platybasia), and/or problems with the bones in the neck.
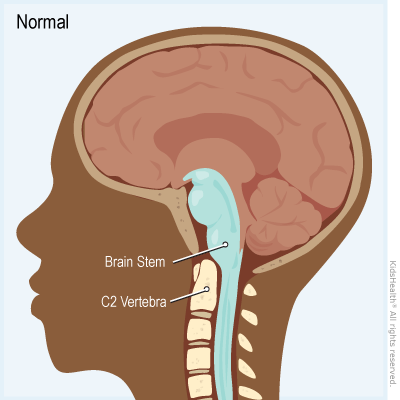
The neck is a stack of separate bones called vertebrae :
- The seven vertebrae in the neck are the cervical vertebrae. They're abbreviated C1–C7.
- C1 sits at the top and supports the skull.
- C2 sits below C1. It has an upright peg at the front that goes up through C1.
- C1 pivots on C2's peg so the head can turn to the right or left.
- Sometimes, that peg pushes up higher than it should, putting pressure on the brainstem.
What Are the Signs & Symptoms of Basilar Invagination?
Basilar invagination can cause different symptoms depending on which part of the brain stem is pinched or pressed. Common symptoms include:
- headache (usually pain in the back of the head or upper neck)
- neck weakness
- nystagmus (twitching eye movements)
- trouble talking or swallowing
- feeling dizzy or lightheaded
- numbness or tingling in the hands or feet
- loss of proprioception (knowing the position of body parts without looking)
- the feeling of a shock down the back when the neck bends forward
- weakness or paralysis of the arms, legs, or both
- trouble going to the bathroom (peeing or pooping), or having pee or poop accidents
Symptoms can get worse when the neck bends forward.
What Causes Basilar Invagination?
A child can be born with the condition (congenital basilar invagination) or develop it over time due to soft bones.
Often, the cause of congenital basilar invagination isn't known. In some babies, it can happen because of conditions such as:
- chiari malformation
- hydrocephalus
- Klippel-Feil syndrome
- syringomyelia (when a fluid-filled cyst forms in the spinal cord)
BI that develops over time can happen because of:
- an injury (such as a fall or car or bike accident)
- a bone, connective tissue , immune, endocrine, or other disorder, such as:
- osteogenesis imperfecta (brittle bone disease)
- Marfan syndrome
- rheumatoid arthritis
- rickets (when bones get soft and weak)
How Is Basilar Invagination Diagnosed?
Children with symptoms of BI are checked by health care providers who specialize in:
- brain and nerve problems (neurology)
- brain and nerve surgery (neurosurgery)
- bone problems (orthopedics)
The provider will ask about symptoms and do an exam, checking muscles and nerves all over the body.
An MRI is the best test to look at the brain stem and spinal cord.
X-rays or a computer tomography (CT) scan also can with diagnosing and assessing basilar invagination.
How Is Basilar Invagination Treated?
Health care providers might just do regular checkups for a child with basilar invagination who has mild or no symptoms.
Some symptoms can be treated with:
- anti-inflammatory medicines
- manual traction (pulling) on the neck
- a cervical (neck) collar or cervical-thoracic brace (which supports the head, neck, and upper back)
- physical therapy
If symptoms include nerve problems or if the neck isn't stable, a child might need surgery. The surgeon may do an operation through the nose, the mouth, or at the back of the head and neck. Sometimes a child needs halo-gravity traction for a few weeks before surgery to help the skull and neck get into a better position.
What Else Should I Know?
As a child with BI grows, be sure to:
- Watch for new or worsening symptoms.
- Go to all follow-up visits as recommended by the health care provider.
- Get any imaging tests needed to check for changes to the skull and neck bones.
Neck injuries in children with basilar invagination are more likely to be severe or fatal than in most children. So they should avoid activities that put them at risk for neck injuries, such as contact sports, diving, and gymnastics.
Reviewed by: Suken A. Shah, MD, Bernadette Fulweiler, APN
Date Reviewed: Jan 20, 2022
















