Pediatric Neurology
Back to NeuroDevelopmental Science Center
We are ranked among one of the best children's hospitals in the country for pediatric neurology and neurosurgery, according to U.S. News & World Report. We combine our expertise of diagnosing and treating disorders of the nervous system with an understanding of childhood medical disorders and the special needs of children and their families.
Department: 330-543-2778
About Neurology
We have the special training and experience to treat your child’s the nervous system problems, working with pediatricians and other primary care doctors as needed. For children with complex or serious medical issues such as epilepsy, their care team may also include behavioral and neuropsychologists, developmental and behavioral pediatricians and pediatric neurosurgeons.
We use a variety of tests and procedures to obtain an accurate diagnosis, such as cerebral angiography, EEG, EMG, nerve conduction velocity testing and transcranial Doppler. We may also use neuropsychological testing to assess cognitive development and function.
We stay up on the latest advances in the treatment of neurologic conditions, such as a ketogenic diet for reducing the number of seizures associated with epilepsy or cognitive behavioral therapy and biofeedback training for managing chronic headaches.
Conditions we diagnose and treat include:
- Seizure disorders, including seizures in newborns, febrile convulsions and epilepsy
- Medical aspects of head injuries and brain tumors
- Weakness, including cerebral palsy, muscular dystrophy and neuromuscular disorders
- Headaches, including migraines
- Behavioral disorders, including attention-deficit/hyperactivity disorder (ADHD), school failure, autism and sleep problems
- Developmental disorders, including delayed speech or motor milestones, and coordination issues
- Intellectual disability
- Hydrocephalus
- Metabolic and mitochondrial diseases
Neurology, Akron
Akron Children's Pediatric Neurology, AkronConsidine Professional Building
215 West Bowery Street
Level 4
Akron, Ohio 44308
Fax: 330-543-8054
Map & directions
More about this location...
Hours
Appointments: 330-543-2778
Department: 330-543-8050
Neurology, Beachwood
Akron Children's Pediatric Neurology, BeachwoodAkron Children's Health Center, Beachwood
3733 Park East Drive
Suite 230
Beachwood, Ohio 44122
Map & directions
More about this location...
Hours
Monday : 8 a.m. - 5 p.m.
Tuesday : 8 a.m. - 5 p.m.
Wednesday : 8 a.m. - 5 p.m.
Thursday : 8 a.m. - 5 p.m.
Friday : 8 a.m. - 5 p.m.
Hours vary by provider and location. Please schedule an appointment online.
Appointments: 330-543-2778
Neurology, Boardman
Akron Children's Pediatric Neurology, Boardman6505 Market Street
Building A
Boardman, Ohio 44512
Fax: 330-729-1144
Map & directions
More about this location...
Hours
Appointments: 330-543-2778
Neurology, North Canton
Akron Children's Pediatric Neurology, North CantonAkron Children's Health Center, North Canton
6076 Whipple Avenue Northwest
North Canton, Ohio 44720
Map & directions
More about this location...
Hours
Appointments: 330-543-2778
Neurology, Medina
Akron Children's Pediatric Neurology, MedinaAkron Children's Health Center, Medina
3778 Medina Road
Medina, Ohio 44256
Map & directions
More about this location...
Hours
Appointments: 330-543-2778
Neurology, Warren
Akron Children's Pediatric Neurology, WarrenThe Market Place
5000 East Market Street
Warren, Ohio 44484
Map & directions
More about this location...
Hours
Monday : 8 a.m. - 5 p.m.
Tuesday : 8 a.m. - 5 p.m.
Wednesday : 8 a.m. - 5 p.m.
Thursday : 8 a.m. - 5 p.m.
Friday : 8 a.m. - 5 p.m.
Saturday : 8 a.m. - Noon
Appointments: 330-543-2778
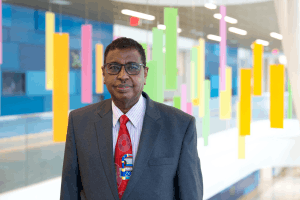
Bruce H. Cohen, MD, FAAN
Director, NeuroDevelopmental Science Center; Philip H. Maynard Chair in NeuroDevelopmental Science Fund; Chairman, American Academy of Neurology Advocacy Committee; Pediatric Neurologist
Michael DiSano, MD
Director, Pediatric Epileptology; Director, Epilepsy Monitoring Unit; Pediatric Epileptologist
Matthew Ginsberg, MD
The James F. and Marguerite A. Pearson Endowed Chair in NeuroDevelopmental Sciences for Rare Diseases; Co-Director, Neurofibromatosis Clinic; Pediatric Neurologist
Lucyna Zawadzki, MD
Director, Ketogenic Diet Program; Pediatric Neurologist/Epileptologist
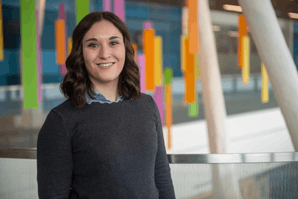
Shawnelle Contini, MSHS, PA-C
Advanced Practice Provider, Inpatient NeuroDevelopmental Science Center
Amanda Delaratta, MSN, APRN-CNP
Advanced Practice Provider, Inpatient NeuroDevelopmental Science Center
Christina Fox-Akers, MSN, APRN-CNP
Advanced Practice Provider, Inpatient NeuroDevelopmental Science Center
Mozhdeh Jucikas, MSN, APRN-CNP
Coordinator, Epilepsy Surgery Program; Pediatric Nurse Practitioner
Open Clinical Studies
Alpers Huttenlocher natural history study (Alpers)
We are conducting this study to understand the history of AHS, a rare genetic disorder that is characterized by seizures, liver dysfunction and progressive developmental regression that leads to early death. Through this study we will determine if there are connections between a patient’s medical history and onset of AHS as well as the relationship between signs and symptoms of presentation of AHS and severity and survival of AHS.
Children born with this disorder will appear heathy at birth and usually develop normally until the onset of their illness. Most patients with AHS will show symptoms of this illness between 2-4 years of age and a smaller group of patients show symptoms for between 17-24 years of age.
For more information on the Alpers-HuttenLocher Syndrome, visit:
https://ghr.nlm.nih.gov/condition/alpers-huttenlocher-syndrome#diagnosis
For complete study information, visit: https://clinicaltrials.gov/ct2/show/NCT03034512?term=alpers-huttenlocher&rank=1
More about this studyNorth American Mitochondrial Disease Consortium Patient Registry and Biorepository (NAMDC)
For complete information, please view the study on clinicaltrials.gov
More about this studySafety and efficacy of Rimegepant for the treatment of migraine in pediatric patients ≥6 to <18 years of age
View complete study information here.
More about this studyStudy of CAP-1002 in Ambulatory and Non-Ambulatory Patients With Duchenne Muscular Dystrophy
For complete information, please visit the study on Clinicaltrials.gov
More about this study