Pediatric Gastroenterology Fellowship
This fellowship works with these departments and clinics:
Colorectal Program, Cystic Fibrosis Center, Gastroparesis Clinic, Motility Program, Myelo Clinic, Eosinophilic Esophagitis Clinic, Gastroenterology
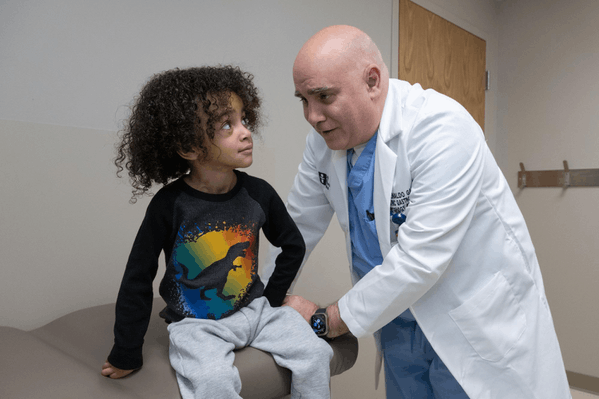
Thank you for taking the time to consider the Akron Children’s pediatric gastroenterology fellowship. Our 3-year, ACGME-accredited Pediatric Gastroenterology Fellowship Program provides exceptional, hands-on clinical training, research opportunities, and academic mentorship to pediatricians seeking to specialize in pediatric gastroenterology, hepatology, and nutrition. Our aim is to prepare fellows to become highly skilled, compassionate pediatric gastroenterologists capable of excelling in clinical care, research, teaching, and leadership roles in diverse healthcare settings.
The ACGME-accredited Pediatric Gastroenterology Fellowship at Akron Children’s Hospital is a 3-year program designed to train the next generation of compassionate, skilled leaders in pediatric gastroenterology, hepatology, and nutrition. Fellows benefit from robust clinical experiences, dedicated research mentorship, and opportunities to teach and lead within a supportive academic environment.
Program Overview
We accept one fellow per year who has completed an accredited pediatric residency. The fellowship spans 36 months and is directed by experienced faculty across clinical, procedural and research domains.
Fellows rotate through Akron Children's in a curriculum designed to progressively build clinical expertise, endoscopic proficiency and scholarly productivity.
Key Training Areas
-
Comprehensive Clinical Training: Fellows develop expertise in diagnosing and managing a wide range of gastrointestinal, liver, and nutritional disorders across all pediatric age groups.
-
Research & Scholarly Activity: Each fellow designs and completes a mentored research project, gaining experience in study design, data analysis, and dissemination.
-
Teaching & Mentorship: Fellows participate in medical education through teaching rounds, case-based learning, and presentations for students, residents, and peers.
-
Leadership & Administration: Involvement in division operations helps fellows build skills in leadership, team coordination, and healthcare systems management.
-
Career Development & Professionalism: Fellows receive personalized mentorship in academic advancement, ethical practice, and preparation for board certification.
Upon completion, fellows will be eligible for American Board of Pediatrics subspecialty certification in Pediatric Gastroenterology, Hepatology & Nutrition and equipped for successful careers in clinical practice, academic medicine, or research.
The following objectives outline the core competencies that fellows will develop throughout the fellowship:
-
Clinical Expertise : Fellows will acquire advanced clinical knowledge and diagnostic skills in pediatric gastroenterology, hepatology, and nutrition: This includes proficiency in the management of common and complex gastrointestinal conditions across a broad spectrum of age groups, including infants, children, and adolescents.
-
Research Skills: Fellows will engage in research activities to develop critical thinking, scientific inquiry, and methodological expertise. Each fellow will identify a research question in either clinical or basic science and will be mentored through the process of formulating a research plan, collecting and analyzing data, and disseminating findings.
-
Teaching and Educational Development: Fellows will develop teaching and mentorship skills through active involvement in educating medical students, residents, and junior fellows. They will prepare and deliver educational presentations, participate in case-based learning sessions, and lead teaching rounds.
-
Leadership and Administrative Skills: Fellows will participate in the administrative functions of the division, including contributing to division meetings, managing the fellows’ conference schedule, and assisting with the coordination of clinical services. This will help fellows develop leadership, team management, and organizational skills necessary for academic or clinical leadership roles.
-
Professionalism and Career Development: Fellows will demonstrate professionalism, ethical behavior, and a commitment to lifelong learning. Fellows will receive mentorship in career development, including guidance on academic promotion, career planning, and preparation for board certification.
Program Completion and Certification: At the conclusion of the three-year fellowship program, fellows will be well-positioned to sit for the American Board of Pediatrics Subspecialty Certification in Pediatric Gastroenterology and Nutrition. They will be expected to have demonstrated mastery in clinical, research, educational, and leadership domains, and to have made substantial contributions to the field of pediatric gastroenterology.
Akron Children’s Pediatric Gastroenterology Department currently has 11 medical staff physicians, and 6 Nurse Practitioners. We complete approximately 3500 procedures per year, including: Upper and Lower Endoscopy with biopsies; Polypectomy; Esophageal Banding; Injection/Sclerotherapy for GI bleeding; Esophageal and Pyloric Balloon dilation. We also regularly perform pH/Impedance Monitoring, Wireless Capsule Endoscopy, and Hydrogen/Methane Breath Testing.
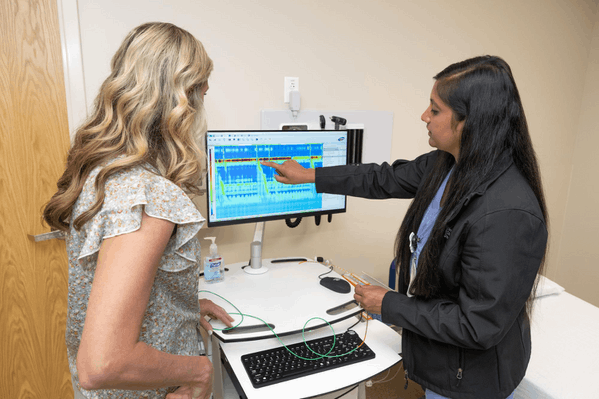
We have an established Motility Program, and regularly perform Anal/Rectal Manometry, Esophageal Manometry (and Endoflip), Full Colonic Manometry, and Antro-Duodenal Motility studies. There is also a dedicated psychology team that works in conjunction with our Functional GI Disorders Clinic. We also work closely with the Pediatric Surgery department with the Bowel Management Clinic.
Akron Children’s GI department is a participant in ICN (Improve Care now). Staff currently participate in the national NASPGHAN (North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition) meeting, as well as multiple other national conventions and poster presentations.
Akron Children’s Pediatric Gastroenterology Department currently has 11 medical staff physicians, 7 Nurse Practitioners, 1 pediatric psychologist, licensed clinical social workers and dietitians. We complete approximately 3500 procedures per year, including: Upper and Lower Endoscopy with biopsies; Polypectomy; Esophageal Banding; Injection/Sclerotherapy for GI bleeding; Esophageal and Pyloric Balloon dilation. We also regularly perform pH/Impedance Monitoring, Wireless Capsule Endoscopy, and Hydrogen/Methane Breath testing
We have an established Motility Program, and regularly perform Anal/Rectal Manometry, Esophageal Manometry (and Endoflip), Full Colonic Manometry, Antro-Duodenal Motility studies and Pelvic Floor Biofeedback. There is also a dedicated psychology team that works in conjunction with our Functional GI Disorders Clinic. We also work closely with the Pediatric Surgery department with the Bowel Management Clinic.
Akron Children’s GI department is a participant in ICN (Improve Care now). Staff are active members of NASPGHAN (North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition) and participate in the annual meeting recurrently, as well as multiple other national conventions and poster presentations.
You must meet the following criteria to apply for our pediatric Gastroenterology, Hepatology and Nutrition fellowship program:
- Completed ERAS application
- MD or DO degree
- Passed all 3 steps of USMLE/COMLEX
- Board-certified/eligible in general pediatrics
- Ohio medical license and DEA number
- U.S. citizenship or J-1 Visa
- 3 letters of recommendation (LOR)
- One LOR must be from your current residency program director
- Advise one LOR should be from Pediatric GI Department Chair
Our fellowship program participates in the National Resident Matching Program (NRMP). You must register for this fellowship by creating an account with NRMP. Contact the NRMP at nrmp@aamc.org or 202-828-0676 with questions.
For more information, contact:
Matthew J. Wyneski, MD
Pediatric Gastroenterology Fellowship Director
Akron Children's
One Perkins Square
Akron, OH 44308
mwyneski@akronchildrens.org
We accept one graduate of an accredited pediatric residency training program each year. Our program's 36-month curriculum and clinical rotation schedule are directed by faculty with expertise in the selected topics.
Fellowship Rotation Structure
PGY-4 (Year 1): Foundational Clinical Year
- Nine blocks of inpatient experience managing consults, admissions, and procedures
- One dedicated outpatient block focused on general and subspecialty clinics
- Two research blocks to begin exploring scholarly interests
PGY-5 (Year 2): Balanced Clinical and Research Year
- Three research blocks to launch a scholarly project with a selected mentor
- Continued exposure to inpatient care, outpatient clinics, and endoscopy
- Two dedicated endoscopy blocks to further procedural independence and deeper outpatient subspecialization
- Core goals: advance research progress and clinical autonomy
PGY-6 (Year 3): Research-Intensive Leadership Year
- Nine research blocks dedicated to completing and publishing a scholarly project
- One outpatient block with opportunities for electives
- Additional endoscopy and inpatient experience to solidify attending-level competence
- Core goals: produce first-author publication, function independently on service, and mentor others
Vacation: 15 days/year
Elective Opportunity: One of the outpatient months of a PGY 6 can be changed to an elective outside rotation
Clinical Sites: All rotations are at Akron Children’s Hospital (ACH) main campus
Clinical Training Highlights
- Inpatient Service (PGY-4 focus): Fellows manage consults, admissions, and procedures. They lead the Pediatric GI resident team and work closely with residents and medical students.
- Outpatient Rotations: Include general GI (16 hrs/wk), eosinophilic esophagitis, cystic fibrosis, hepatology, motility, and constipation/biofeedback clinics.
- Endoscopy Training: Begins in PGY-5 and continues into PGY-6 with progressive independence.
- Transnasal Endoscopy experience available.
Scholarly Activity
- PGY-4: Focus is on identifying interests and project ideas.
- PGY-5–6: Fellows select a mentor and develop a clinical, translational, or laboratory-based project.
- Goal: Complete a first-author publication in a peer-reviewed journal by the end of fellowship.
Didactics & Conferences
Fellows participate in a robust educational curriculum:
- Weekly: Core topic lectures (12-month cycle), Pediatric GI conferences
- Monthly:
- Interdisciplinary GI conference
- Board review
- Pathology conference
- Case conference
- Journal club (fellow-led)
Additional Details
- Scholarly Oversight: Guided by the Program Director and faculty mentors
- Total Research Blocks: 14 months
- PGY-4: 2 blocks
- PGY-5: 3 blocks
- PGY-6: 9 blocks
- Moonlighting: Not permitted at any fellowship year per ACGME and program policy
Members of our faculty are distinguished in a variety of fields including neurogastroenterology & motility, hepatology, cystic fibrosis, transnasal endoscopy, clinical informatics, improvement science, medical education and hospital administration.
Click here to view the faculty of the gastroenterology program.
Akron Children’s accredited fellowship programs offer:
Stipends
(Effective July 1, 2025)
PL-4 – $75,794
PL-5 – $77,309
PL-6 -- $78,856
Vacation
House offices are granted 3 weeks of vacation or 15 customary working days.
Conference Time
Fellows are entitled to 5 days of conference time each year for medical conventions and courses outside the hospital.
Educational Allowance
Fellows are provided $1,500 annually for use toward medical-related journals or books, conferences, and license renewals.
Research and Scholarship Travel
The Department of Pediatrics encourages and supports investigator-initiated research by subspecialty fellows. Therefore, the Department supports research-related travel when the fellow is in good academic and professional standing, and when prior written approval of the program director is documented. All hospital policies relating to travel must be followed.
Although the policy relates to presentation at a national forum, requests for support for presentation at a regional forum are considered on a case-by-case basis.
Additionally, funding may be available to offset costs for professional conferences (travel, lodging, registration, meals) if not presenting scholarly activity.
Professional Liability
Professional liability insurance is provided by the hospital.
Health Benefits
Fellows, and their dependents, are eligible to enroll in the hospital’s health, dental, and vision insurance programs. Costs are shared between the fellow and the hospital. Benefits are available immediately.
Retirement Benefits
Fellows may participate in the Hospital’s 403(b) Plan from their date of hire. Match dollars are not available to fellows.
Other Benefits
- Group Term Life Insurance equal to one time the fellow’s annual income, with an option to purchase additional coverage in increments of annual earnings.
- Dependent Life Insurance coverage and Medical Dependent Care Flexible Spending Accounts.
- Voluntary Universal Life, Accident & Critical Illness through Trustmark & Home& Auto through Met Life.
- Employee Assistance Program available to all fellows and their families.
- Short and Long Term Disability benefits available, effective for three months following start date.
Medical License & DEA
Fellows are required to obtain an Ohio State Medical License and DEA certificate prior to beginning training.
Parking
A key access card for convenient parking is provided at no charge.
Lab Coats
One embroidered lab coat is provided, if desired.
Meals
Fellows are given $70 every week for use in the hospital cafeteria.
Relocation expenses
The hospital provides reimbursement for initial relocation expenses, up to $1,000, subject to current tax laws.
Smoke, Electronic Cigarette and Tobacco Free Campus
Akron Children’s is a tobacco-free healthcare system. Prospective employees who test positive for nicotine will have their offer of employment rescinded and will not be permitted to start work.
Hopkins LC, Holloman C, Webster, A, Labyk AN, Penicka C, May L, Sharn A, Gupta S, Schier H, Kennel JA, Gunther C. Caregiver Diet and Health Outcomes of the Simple Suppers Program: A 10-week, 2-group Quasi-Experimental Family Meals Trial. Nutrients. 2022;14(250). https://doi.org/10.3390/nu14020250
Gupta SR, Mezoff E, Dienhart M. Lead Toxicity from a Swallowed Fishing Sinker: A Case Report. JPGN Report. 2021 Aug;2(3):p e084. doi: 10.1097/PG9.0000000000000084
Gupta S, Baaleman DF, Benninga MA, Bali N, Vaz K, Yacob D, Di Lorenzo C, Lu PL. The use of linaclotide in children with functional constipation or irritable bowel syndrome: a retrospective review. Paediatr Drugs. 2021 Apr 20. doi: 10.1007/s40272 021-00444-4.
Hawa K, Gupta S, Saps M. Abdominal migraines: Variations in diagnosis and care between pediatric gastroenterologists and neurologists. Rev Chil Pediatr. 2020;91(1): 46 50.
Gupta SR, Crandall WV, Donegan A, Johnson M, Drobnic B, Oates M, Boyle B, Maltz R, Dotson JL. A Quality Improvement Approach to External Infliximab Infusions in Pediatric Inflammatory Bowel Disease. J Pediatr Gastroenterol Nutr. 2019 Nov;69(5):544-550.
Gupta S, Schaffer G, Saps M. Pediatric irritable bowel syndrome and other functional abdominal pain disorders: an update of non pharmacological treatments. Expert Rev Gastroenterol Hepatol. 2018 May;12(5):447 456.
Saps M, Gupta SR. Functional abdominal pain disorders in children: An update on treatment. NeuroGastroLatam Rev. 2017;1:206-214.
Gupta SR, Wolf K. Right Lower Quadrant Pain and Osteopathic Manipulative Medicine: A Case Report. ACOP Ejournal. 2017: EJOURNAL-D-17-00007.
Remien KA, Moore R, Son E, Watson K, South AP. Recurrent Abdominal Distention in a 5-Week Old Full-Term Infant. Clinical Pediatrics (Phila). 2023;99228231191591. doi:10.1177/00099228231191591
Remien K, Mancuso M, Watson K. Pediatric Collagenous Gastroenteritis and Colitis Presenting as Protein-Losing Enteropathy. ACG Case Reports Journal 10(4):p e01028, April 2023. doi: 10.14309/crj.0000000000001028
Lambert-Jenkins, K; Rossman, I; Watson, K. Treatment of Inflammatory Bowel Disease and Pediatric Onset Multiple Sclerosis with Ocrelizumab and Ustekinumab in a JC-virus Positive Adolescent. JPGN Reports. 2022 Aug; 3(3): p e214 doi: 10.1097/PG9.0000000000000214
Watson K, Kim SC, Boyle BM, Saps M. The prevalence and impact of functional abdominal pain disorders in children with inflammatory bowel diseases (IBD-FAPD). Journal of Pediatric Gastroenterology and Nutrition. 2016 Nov; doi: 10.1097/MPG.0000000000001479.
Creation of a neopylorus after pyloric exclusion using a "double-endoscope" technique. Gibbons AT, Bruns NE, Garcia R, Wyneski MJ, Ponsky TA - - Surg Endosc. 2016 Jul;30(7):3133-7
Endoscopic Web Localization for Laparoscopic Duodenal Web Excision. Bruns NE, Gibbons AT, Wyneski MJ, Ponsky TA. - - Surg Laparosc Endosc Percutan Tech. 2015 Dec;25(6):e172-4.
Chen CB, Mistry N, Zeft A, Garcia-Naveiro R, Hupertz V, Hashimoto K, Radhakrishnan K. Rare genetic mutation triggering acute liver failure in a toddler requiring a liver transplant. Pediatric Transplantation. June 2021/volume 25, Issue 6/ e 14048.
Singh P, Garcia R, Phadke M. Neuromyelitis Optica spectrum disorder manifested by persistent hiccups and severe esophagitis in an adolescent patient. 2021 Nov. JPGN reports. Volume 2 – issue 4 – p e177.
DiMaggio, DM., Du, N., Scherer, C., Brodlie, S., Shabanova, V., Belamarich, P., Porto, AF. Comparison of Imported European and US Infant Formulas: Labeling, Nutrient, and Safety Concerns. J Pediatr Gasroenterol Nutr. 2019 May 9.
Scherer C, Sosensky P, Schulman-Green D, Levy M, Smith C, Friedlander J, Koral A. Pediatric Patients' and Parents' Perspectives of Unsedated Transnasal Endoscopy in Eosinophilic Esophagitis: A Qualitative Descriptive Study. J Pediatr Gastroenterol Nutr. 2021 Apr 1;72(4):558-562. doi: 10.1097/MPG.0000000000003029. PMID: 33394888.
Phatak, U., Scherer, C., Du, N., Friedlander, J. Pediatric Web-based Video Capsule Endoscopy Curriculum: A Pilot Study to Determine the Ability to Implement a Standardized Educational Curriculum, JPGN Reports: February 2022 – Volume 3 – Issue 1 – p e130 doi:10.1097/PG9.0000000000000130
Vespoli CN, Iqbal AM, Kabbany NM, Radhakrishnan KR. Metabolic-Associated Fatty Liver Disease in Childhood and Adolescence. 2023 Sep;52(3):417-430. doi: 10.1016/j.ecl.2023.02.001. Epub 2023 Mar 16; PMID: 37495334
Seif Pasquarella, C., Kaplan, B., Mahajan, L., Lamparyk, K., Kay, M. "A Single Center Review of Pediatric Colonoscopy Quality Indicators." J Pediatr Gastroenterol Nutr. 2019 May;68(5):648-654. doi: 10.1097/MPG.0000000000002239 PMID: 30562311
By using this site, you consent to our use of cookies. To learn more, read our privacy policy.