Massillon native Julia Bonner poses with her fiancé and 3 healthy, active children: Julian, 10, Isabella, 2, and Arianna, 6 months. Julia underwent 18 life-saving intrauterine blood transfusions to treat her babies for fetal anemia.
For Julia Bonner, it was just another routine prenatal testing appointment. Yes, the Massillon native pregnant with her first child had all the common pregnancy discomforts (and swollen ankles), but there was no cause for concern. Her baby boy was growing and developing as expected.
It wasn’t until her Red Blood Cell (RBC) Antibody screen came back positive that everything changed. Julia was diagnosed with a rare condition called alloimmunization, which occurs when a person’s immune system produces RBC antibodies after exposure to a foreign blood type. While unknown, it’s possible this exposure happened during birth when Julia’s blood mixed with her mother’s.
RBC antibodies attack and destroy foreign red blood cells (i.e., an unborn baby with a different blood type than its mother) as protection. They can cross the placenta and cause Julia’s unborn baby’s red blood cells to break down, leading to severe, life-threatening anemia. Without red blood cells, her baby wouldn’t receive the oxygen he needed to grow and thrive.
“Because I had a negative blood type, my doctor knew I’d have complications in my pregnancy, but we didn’t know to what extent,” Julia said. “It was definitely scary to get these test results. I didn’t know how it would affect my son now and what the outcome would be later on.”
Julia was referred to Akron Children’s Maternal-Fetal Medicine for ongoing testing and monitoring to ensure Julia’s baby wasn’t growing anemic.
Katherine Wolfe, DO, a maternal-fetal specialist at Akron Children’s, performed an ultrasound on Julia every 1 or 2 weeks, depending on baby’s condition, to measure blood flow in his brain and check for anemia.

All of Julia’s babies spent time in Akron Children’s NICU after delivery for ongoing care. Arianna (pictured) was delivered at 32 weeks and spent 6 weeks in the NICU, where she received 2 more blood transfusions.
By Julia’s third trimester, anemia was suspected. After sampling baby’s blood from the umbilical cord under ultrasound guidance to confirm the diagnosis, Dr. Wolfe and her team performed an intrauterine blood transfusion through the umbilical cord to treat his anemia.
“An intrauterine blood transfusion uses donated blood that does not have the specific antigens that Julia’s antibodies destroy,” explained Dr. Wolfe. “These transfused cells will eventually break down, but not as fast as the baby’s natural red blood cells. That is why transfusions are repeated frequently during pregnancy to allow baby to develop.”
Julia underwent 2 more intrauterine blood transfusions with her son, Julian; 6 with her second child, Isabella; and 9 with her third child, Arianna.
“Each pregnancy got more severe and complicated. The antibodies got stronger,” Julia said. “Dr. Wolfe was amazing, and I’m so grateful she was here to do these procedures with all of my kids. She’s so personable, answered all of my questions and made sure I could get ahold of her at any time. She’s absolutely incredible.”
Julia’s second pregnancy required more care and the intrauterine blood transfusions came earlier. They began in her second trimester, as opposed to the third with Julian.
By her third pregnancy, Julia’s baby became anemic in the first trimester. Unfortunately, it’s not possible to perform an intrauterine blood transfusion until at least 16 weeks due to baby’s tiny size.
By that time, Arianna was severely anemic and required a life-saving blood transfusion. Doctors gave her a 10% chance of survival. She was still too small to transfuse through the umbilical cord. Instead, Dr. Wolfe, along with Abdelaziz Saleh, MD, PhD, division director of Akron Children’s Fetal Treatment Center, transfused blood through Arianna’s belly in utero. They had to do this procedure 3 times until Arianna reached 20 weeks and doctors could then transfuse blood through the umbilical cord.
“Arianna developed anemia at a very early gestational age, which vastly increased the risk of procedure-related complications,” said Dr. Wolfe. “Plus, she had to undergo that many more procedures during the pregnancy because her anemia began so early in gestation.”

Arianna underwent 9 intrauterine blood transfusions and was given a 10% chance of survival. Today, she’s a happy, healthy baby eager to crawl to keep up with her older siblings.
Ongoing care after birth
After birth, all 3 of Julia’s babies spent time in Akron Children’s Neonatal Intensive Care Unit (NICU) for ongoing care, oxygen support and hemoglobin monitoring.
Julian was born at 35 weeks and spent 5 weeks in the NICU. He was born with severe anemia, and his bilirubin levels were so high that he required an exchange blood transfusion, which removed Julian’s blood and replaced it with donated blood.
“Julian’s liver was having a hard time processing all the dead red blood cells, so he had severe jaundice, too,” said Julia. “The exchange transfusion was necessary to thin the population of antibodies that were attacking his red blood cells. It can take a few weeks after birth to clear them out. Luckily, the exchange transfusion worked.”
Thankfully, Julia’s daughters didn’t require an exchange transfusion. Isabella was delivered at 32 weeks and spent 8 weeks in the NICU. She had 3 blood transfusions before she was released for home.
Arianna also was delivered at 32 weeks and spent 6 weeks in the NICU. She required 2 blood transfusions.
Once released for home, Julia’s babies were monitored by doctors in Akron Children’s pulmonary and hematology departments for several months. Doctors monitored hemoglobin levels by doing complete blood counts to ensure red blood cells were maintaining and weren’t dropping, and the babies were thriving.
“Thankfully, Arianna is a fighter and did great with the procedures and is now healthy and thriving,” said Julia. “Doctors took very good care of her, were so knowledgeable and got her through that initial anemia stage so early in my pregnancy. I’m thrilled she’s off oxygen completely and hasn’t had a blood transfusion in months. We’re hoping she’ll be released from hematology care soon.”
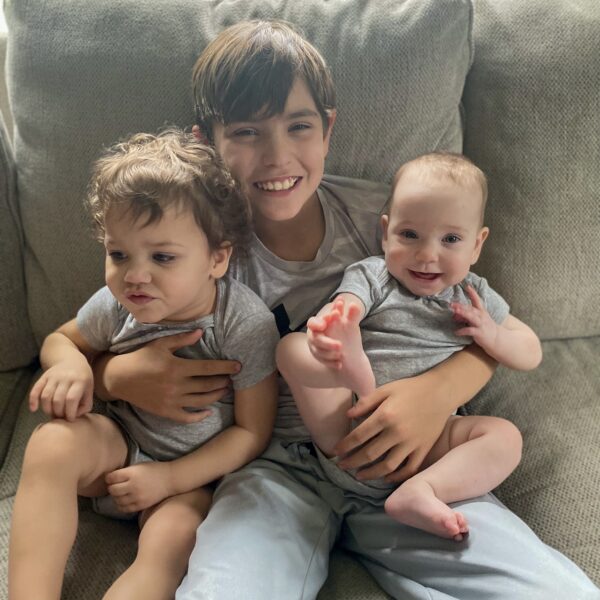
Once born, Julian (center) required a life-saving exchange blood transfusion to treat severe jaundice and thin the population of antibodies that were attacking his red blood cells.
Today, Julia’s 3 kids are healthy and active. Julian, 10, is an honor roll student and enjoys playing sports. He’s a gray belt in jiujitsu and trains year-round, in addition to playing baseball and football. Isabella, 2, is a climber and loves being active. In sporadic calm moments, she enjoys coloring and watching Disney’s Encanto. Arianna, 6 months, is meeting her milestones and starting to crawl to keep up with her siblings.
“I’m so thankful for the doctors’ vast knowledge on how to take care of my babies and get them what they needed,” said Julia. “Their knowledge and what they can do blows my mind. I thank God for them. Without medical technology, I wouldn’t have any of my children. I can’t describe how grateful I am for the doctors and nurses at Akron Children’s.”
Learn more about Akron Children’s Maternal-Fetal Medicine. To schedule an appointment, call 330-543-4500.