
David had his first heart procedure the afternoon he was born.
To look at David Campbell of Brimfield, Ohio, you’d see a 6-month-old with expressive eyes and a big smile. You’d never know he needed multiple heart interventions – the first within hours of being born – to save his life.
More than a decade ago, Akron Children’s and Cincinnati Children’s joined forces to provide specialized care for patients in need of kidney transplants. The relationship expanded in 2024 to include complex care for ear, nose and throat (ENT) conditions, liver disease and bone marrow transplants. The two health systems added cardiology and cardiothoracic surgery in 2025, bringing world‑class congenital heart surgery and cardiac care closer to home for patients and families in the Akron area.
Diagnosis, planning and immediate intervention
Life took an unexpected turn for David’s parents, Bethany and Jimmy, at the 20-week ultrasound. “They found an issue with David’s heart,” Bethany recalled. “We knew that he would have a serious heart defect and may be too sick for treatment.”
Akron Children’s Heart Center cardiovascular surgeon Dr. Tara Karamlou, who serves as the joint program surgeon for the Akron Children’s and Cincinnati Children’s heart collaboration, met with Bethany and Jimmy on the day of David’s diagnosis. “It’s the worst day of your life when you get such devastating news about your baby,” Bethany said. “Getting to meet with Dr. Karamlou that day and hear her optimism was amazing.”
Interventional cardiologist Dr. Ari Gartenberg and Dr. Karamlou saw David prenatally. They also discussed David’s case with their colleagues at the Cincinnati Children’s Heart Institute.
David’s diagnosis of “hypoplastic left heart syndrome (HLHS)” means the left side of the heart is underdeveloped and does not pump blood to the rest of the body. He had an additional complication – a “restrictive atrial septum” – which would require a heart catheterization immediately after birth. Then, he’d need a series of surgeries to give him a chance to live.

Bethany and Jimmy relied on faith and family to get through challenging times.
David entered the world Aug. 2, 2025, at 9 a.m. at Summa Health. An ambulance transported David and Jimmy to Akron Children’s 3 hours later, while Bethany recovered at the hospital.
That afternoon, David needed an emergency “atrial septostomy” procedure to improve blood flow between the 2 upper chambers of his heart. He needed it to save his life and stabilize him for open-heart surgery. “Bethany got a day pass from Summa and came to Akron Children’s to see David,” Jimmy said. “I baptized him in the pediatric intensive care unit (PICU) before the procedure, which was very special.”
The next morning, David flew to Cincinnati Children’s in the Akron Children’s medical helicopter.
Specialized surgery
At 5 days old, David had open-heart surgery in Cincinnati. “David’s left ventricle couldn’t do the job of pumping oxygenated blood to the body because it was too small,” said Dr. David Morales, executive co-director of the Cincinnati Children’s Heart Institute. “As a result, we performed the Norwood procedure on him.
“We put the aorta, which usually takes blood rich in oxygen to the rest of the body, with the lung artery. This newer, larger neo-aorta now goes from the right ventricle to the body. We also used a shunt, a tube that connects the right ventricle to the lung arteries, to take blood to David’s lungs.”
David returns to Akron Children’s and a second surgery
He spent 2 weeks at Cincinnati Children’s, recovering from surgery. He came off the ventilator days faster than most babies, and his family was relieved he responded so well. David returned to the Akron Children’s PICU to continue his recovery – and he finally went home in late August.
David is the first grandchild on either side of the family, and everyone wanted to meet him. “We needed to keep our high-risk baby safe, but we didn’t want his entire life to be spent in a doctor’s office,” Jimmy said. “Our immediate family and friends got to meet him. We did fall activities including taking David to the zoo, the apple orchard and on walks – so he could be outside and away from crowds.”
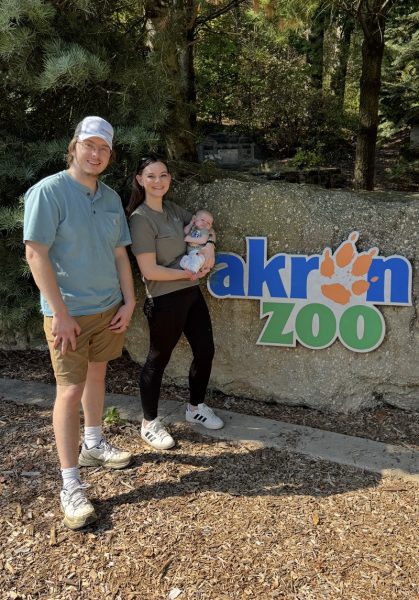
Between surgeries, Jimmy and Bethany took David on hikes, walks and trips to the zoo.
The Norwood procedure kept him alive until he grew enough to have a second surgery – the Glenn procedure – at Akron Children’s in early December. “Glenn is an intermediate surgery for babies with HLHS and other single-ventricle heart defects,” Dr. Karamlou explained. “We removed the shunt from the Norwood procedure, creating a direct connection to the lungs to improve oxygen levels and reduce the workload of David’s single ventricle.”
David did well after the Glenn procedure, and the cardiology team is pleased with the function of his heart. He’ll have another heart surgery, called the Fontan procedure, around ages 3 to 5. “He’s been a rock star,” Bethany said. “Jimmy and I are back to work – and we’re doing ‘normal’ things like planning play dates for David.”

At 6 months, David is growing and thriving.
Looking back
For Dr. Karamlou, a patient like David highlights the strength of the Akron Children’s and Cincinnati Children’s partnership. “It provides opportunities for collaborative learning, as we share expertise and innovative ideas,” she said. “We make both programs better, and our patients receive world-class care.”
Learn more about the Akron Children’s Heart Center.










