
It’s been an eventful year for Liz and Jake Balizet, as Garrett had his second open-heart surgery in February and Mason arrived in July.
Liz Balizet of Navarre, Ohio didn’t realize the great pediatric care that’s available in northeast Ohio until her first child was diagnosed with a complex heart condition.
Liz’s 20-week ultrasound showed problems with her baby boy’s heart. She and her husband, Jake, received a referral to the Akron Children’s Heart Center. “We went out to the truck and just cried because of the unknown,” she recalled. “I closed baby Garrett’s nursery door when we got home, not even being able to go in or look at it. I wasn’t sure we were going to be bringing a baby home to it.”
Liz switched her prenatal care to Akron Children’s Maternal-Fetal Medicine and started seeing Cardiologist Dr. Chandrakant Patel for monthly tests to monitor Garrett’s heart. “It’s important to be compassionate when you are in those difficult circumstances; that’s the ‘art’ of medicine,” Dr. Patel said. “We have to look into the parents’ eyes, and you feel it when you share bad news that their child has a heart problem.”
Garrett’s right ventricle was smaller than it should be. His “tricuspid valve,” which helps blood flow from the right atrium to the right ventricle, was missing. And he had a hole between the right and left ventricles. He would need multiple open-heart surgeries.
Dr. Patel consulted with Dr. Robert Stewart, who would perform Garrett’s surgeries. “In situations like Garrett’s, we talk to the surgical team before the baby is even born,” Dr. Patel explained. “Then we meet with the family, so they can get acquainted with the surgeon who will be taking care of their baby.”

Garrett loves to be in motion, whether riding his bike or a kids’ tractor.
Garrett arrives
Liz delivered Garrett via Cesarean section at Summa Health on May 29, 2021. “I only got to hold him for a few minutes,” she said. “Then, he got transferred to the Akron Children’s Neonatal Intensive Care Unit (NICU).”
Garrett spent 9 days in the NICU. He did so well that he didn’t need the first heart surgery, like most babies with his condition. “At home, we had to check his weight and the oxygen saturation in his blood daily. We also had to log how long he ate and how much,” Liz said. “Monitoring Garrett’s information was so stressful, especially as first-time parents.”
Garrett has two heart surgeries
Most babies with Garrett’s condition have surgery around 6 months old. He ate so well and grew so much that his heart couldn’t keep up with the rest of his body, so he has the first surgery just shy of 3 months old.
The right side of your heart normally sends blood to the lungs to get oxygen – while the left side sends oxygen-rich blood to the rest of the body. In babies like Garrett who have a right ventricle that’s too small, the left side has to send blood to the lungs and the body. The Glenn surgery Garrett had changed the blood flow, so blood from his upper body goes straight to his lungs. This way, the single working side of his heart only sends blood to the body and doesn’t have to work as hard.
Garrett recovered well, only spending 4 days in the hospital. Liz and Jake no longer had to monitor Garrett’s weight, feeding and oxygen levels. His oxygen saturation was 75-80% – lower than the usual 95-100% for a child – so he couldn’t walk far or do much without getting out of breath. They reassured him of the things he’d be able to do after his second surgery, the Fontan procedure.
He had the Fontan surgery in February 2025. This procedure reroutes blood flow, bypassing Garrett’s small right ventricle to send oxygen-poor blood directly to his lungs for oxygenation without passing through his heart.
Dr. Patel checked in with Liz and Jake when Garrett had his surgeries. “Even though Dr. Stewart performed the surgeries, I stopped by the waiting room and talk to the family,” Dr. Patel shared. “Having their cardiologist visit while their child is in surgery is part of building a good relationship with the family.”

Two thumbs up for Garrett before his Fontan heart procedure in February.
A special heart
Since the Fontan surgery, Garrett’s oxygen saturation has climbed to 95-96%. “That surgery was truly a life-changer,” Liz said. “Garrett has more energy than I’ve ever seen. He runs around all the time, rides his bike, keeps up with his friends, plays T-ball and loves to dig in the dirt.”
He also has an important, new role: big brother. “When I was pregnant, Garrett constantly hugged and kissed on my belly,” Liz shared. “Now, he wants to hold, hug and kiss baby Mason all the time. Garrett tells us all the things he’s going to teach Mason one day.”
Garrett knows his heart is special. “He’ll show anyone his chest scar, and he thinks it’s the coolest thing,” Liz said. “No additional heart surgeries are planned, but he will need a transplant someday. We’re encouraged that as medicine advances, 30 to 40 years from now, a heart transplant will be comparable to a pacemaker surgery today.”
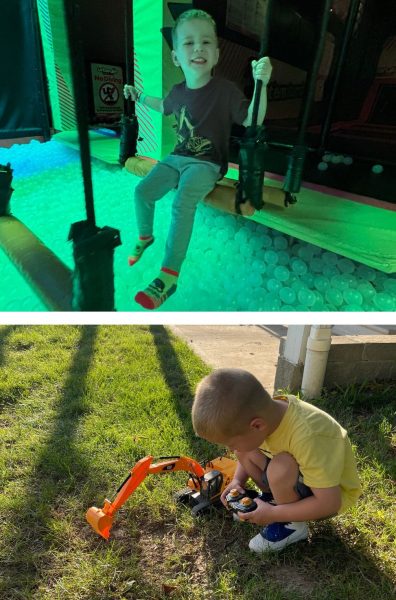
Garrett now has more energy to swing, dig in the dirt and enjoy being a kid.
Many providers and loved ones to thank
As Liz looks back, she’s thankful to Akron Children’s team for making Garett’s experience as good as it could be under the circumstances. “Drs. Patel, Stewart and Khan were great every step of the way,” she said. “Nurse Practitioner Kathryn Wheller makes sure we have all our questions answered, no matter how silly they may be.”
Liz and Jake also have a strong support system at home. “Our parents have been such a blessing. We also have grandparents, aunts, uncles and cousins who would drop anything to help us,” Liz said. “Jake works for an amazing, family-owned company who has been so understanding when he needs time off. We have such a huge village; I can’t even put into words how grateful we are to have them.”
Similar stories:
Julien creates his own superheroes to help him stay strong against kidney disease
Dr. Anton Milo answers your questions on ear tube surgery
Akron Children’s Mahoning Valley begins construction and renovation to inpatient units
Build Healthy Bones to Reduce Stress Fracture Risk
After skull reconstruction, Fitz’ brain has room to grow
Learn more about the specialized care in Maternal-Fetal Medicine and the Heart Center.










